What Is Cancer?
In the most basic terms, cancer refers to cells that
grow out-of-control and invade other tissues. Cells may become cancerous due to
the accumulation of defects, or mutations, in their DNA. Certain inherited
genetic defects (for example, BRCA1 and BRCA2 mutations) and infections can
increase the risk of cancer. Environmental factors (for example, air pollution)
and poor lifestyle choices—such as smoking and heavy alcohol use—can also
damage DNA and lead to cancer.
Most of the time, cells are able to detect and repair
DNA damage. If a cell is severely damaged and cannot repair itself, it usually
undergoes so-called programmed cell death or apoptosis. Cancer occurs when
damaged cells grow, divide, and spread abnormally instead of self-destructing
as they should.
Malignant Tumors Vs. Benign Tumors
A tumor is an abnormal mass of cells. Tumors can either be benign (non-cancerous) or malignant (cancerous).>> Benign Tumors
Benign tumors grow locally and do not spread. As a result, benign tumors are not considered cancer. They can still be dangerous, especially if they press against vital organs like the brain.>> Malignant Tumors
Malignant tumors have the ability to spread and invade other tissues. This process, known as metastasis, is a key feature of cancer. There are many different types of malignancy based on where a cancer tumor originates.Cancer Metastasis
Metastasis is the process whereby cancer cells break free from a malignant tumor and travel to and invade other tissues in the body. Cancer cells metastasize to other sites viaWhat Causes Cancer?
Certain genes control the life cycle—the growth, function, division, and death—of a cell. When these genes are damaged, the balance between normal cell growth and death is lost. Cancer cells are caused by DNA damage and out-of-control cell growth. The following is a partial list of factors known to damage DNA and increase the risk of cancer:Mutations Cause
Environment Cause
Cancer may be caused by environmental exposure. Sunlight can cause cancer through ultraviolet radiation. So can air pollutants like soot, wood dust, asbestos, and arsenic, to name just a few.
Microbes Cause
Some microbes are known to increase cancer risks. These include bacteria like H. pylori, which causes stomach ulcers and has been linked to gastric cancer. Viral infections (including Epstein-Barr, HPV, and hepatitis B and C) have also been linked to cancer.
Lifestyle and Diet Causes
Lifestyle choices can lead to cancer as well. Eating a poor diet, inactivity, obesity, heavy alcohol use, tobacco use including smoking, and exposure to chemicals and toxins are all associated with greater cancer risk.
Causes of Cancer: Treatment
Medical treatment with chemotherapy, radiation, targeted treatments (drugs designed to target a specific type of cancer cell) or immunosuppressive drugs used to decrease the spread of cancer throughout the body can also cause damage to healthy cells. Some “second cancers”, completely separate from the initial cancer, have been known to occur following aggressive cancer treatments; however, researchers are producing drugs that cause less damage to healthy cells (for example, targeted therapy).Cancer Symptoms and Signs
There are more than 100 different types of cancer. Every cancer and every individual is unique. Cancer symptoms and signs depend on the size and location of the cancer as well as the presence or absence of metastasis.- Fever
- Pain
- Fatigue
- Skin changes (redness, sores that won't heal, jaundice, darkening)
- Unintended weight loss or weight gain
Other more obvious signs of cancer may include:
- Lumps or tumors (mass)
- Difficulty swallowing
- Changes or difficulties with bowel or bladder function
- Persistent cough or hoarseness
- Short of breath
- Chest pain
- Unexplained bleeding or discharge
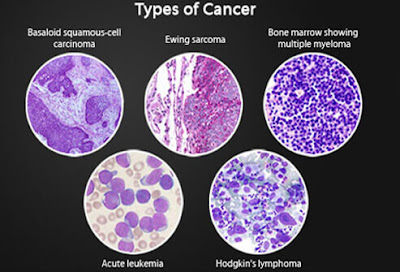
6 Types of Cancer
Cancer can occur anywhere in the body. Broadly, cancers are classified as either solid (for example breast, lung, or prostate cancers) or liquid (blood cancers). Cancer is further classified according to the tissue in which it arises.1. Carcinoma
Carcinomas are cancers that occur in epithelial tissues in the body. They comprise 80% to 90% of all cancers. Most breast, lung, colon, skin, and prostate cancers are carcinomas. This class includes the two most common skin cancers, basal cell carcinoma and squamous cell carcinoma. Also in this class is the glandular cancer adenocarcinoma.2. Sarcoma Cancer
Sarcomas occur in connective tissue like the bones, cartilage, fat, blood vessels, and muscles. This class of cancers includes the bone cancers osteosarcoma and Ewing sarcoma, Kaposi sarcoma (which causes skin lesions), and the muscle cancers rhabdomyosarcoma and leiomyosarcoma.3. Myeloma Cancer
Myelomas are cancers that occur in plasma cells in the bone marrow. This class of cancer includes multiple myeloma, also known as Kahler disease.4. Leukemia
Leukemias are a group of different blood cancers of the bone marrow. They cause large numbers of abnormal blood cells to enter the bloodstream.5. Lymphoma Cancer
Lymphomas are cancers of the immune system cells. These include the rare but serious Hodgkin lymphoma (Hodgkin’s lymphoma, also Hodgkin’s disease) and a large group of white blood cell cancers known collectively as non-Hodgkin lymphoma (non-Hodgkin’s lymphoma).6. Mixed Cancer
Mixed cancers arise from more than one type of tissue.
How Stages of
Cancer Are Determined
Doctors use the stages of cancer to classify cancer
according to its size, location, and extent of spread. Staging helps doctors
determine the prognosis and treatment for cancer. The TNM staging system
classifies cancers according to:
- Tumor (T): Primary tumor size and/or extent
- Nodes (N): Spread of cancer to lymph nodes in the regional area of the primary tumor
- Metastasis (M): Spread of cancer to distant sites away from the primary tumor
Some cancers, including those of the brain, spinal
cord, bone marrow (lymphoma), blood (leukemia), and female reproductive system,
do not receive a TNM classification. Instead, these cancers are classified
according to a different staging systems.
What Are The
Stages of Cancer?
The TNM classification of a cancer usually correlates
to one of the following five stages.
- Stage 0: This refers to cancer that is "in situ," meaning that cancerous cells are confined to their site of origin. This type of cancer has not spread and is not invading other tissues.
- Stage I – Stage III: These higher stages of cancer correspond to larger tumors and/or greater extent of disease. Cancers in these stages may have spread beyond the site of origin to invade regional lymph nodes, tissues, or organs.
- Stage IV: This type of cancer has spread to distant lymph nodes, tissues, or organs in the body far away from the site of origin.
Diagnosing Cancer
Various tests may be performed in order to confirm a cancer diagnosis. Positron Emission Tomography and Computed Tomography (PET-CT) Scans and other similar tests canThe most common test and procedures used to diagnose cancer include:
- Mammogram
- Pap Test
- Tumor Marker Test
- Bone Scan
- MRI
- Tissue Biopsy
- PET-CT Scan
The Role of Lymph Nodes in Cancer Diagnosis
 Cancer that originates in the
lymph nodes or other area of the lymphatic system is called lymphoma. Cancer
that originates elsewhere in the body can spread to lymph nodes. The presence
of metastasized cancer in the lymph nodes is may mean the cancer is growing
quickly and/or is more likely to spread to other sites. The presence of cancer
in lymph nodes often affects prognosis and treatment decisions. Many diagnostic
tests look at the lymph nodes as an indicator.
Cancer that originates in the
lymph nodes or other area of the lymphatic system is called lymphoma. Cancer
that originates elsewhere in the body can spread to lymph nodes. The presence
of metastasized cancer in the lymph nodes is may mean the cancer is growing
quickly and/or is more likely to spread to other sites. The presence of cancer
in lymph nodes often affects prognosis and treatment decisions. Many diagnostic
tests look at the lymph nodes as an indicator. What Are Treatment Options?
The treatment is highly variable depending on the type and stage of a cancer as well as the overall health of the patient. The most common treatments are surgery, radiation, and chemotherapy. Other treatments include targeted/biological therapies, hematopoietic stem cell transplants, angiogenesis inhibitors, cryosurgery, and photodynamic therapy.Every treatment has potential risks, benefits, and side effects. The patient and his or her care team, which may include an internist or other specialist, surgeon, oncologist, radiation oncologist, and others, will help determine the best and most appropriate course of treatment.
Until a cure can be found, prevention through a healthy lifestyle is the best way to stop cancer. Some ways to help protect yourself from cancer include eating plenty of fruits and vegetables, maintaining a healthy weight, abstaining from tobacco, drinking only in moderation, exercising, avoiding sun damage, getting immunizations, and getting regular health screenings.
Surgery
Sometimes, cancer cannot be entirely surgically removed because doing so would damage critical organs or tissues. In this case, debulking surgery is performed to remove as much of the tumor as is safely possible. Similarly, palliative surgery is performed in the cases of advanced cancer to reduce the effects (for example, pain or discomfort) of a cancerous tumor. Debulking and palliative surgeries are not curative, but they seek to minimize the effects of the cancer.
Reconstructive surgery can be performed to restore the look or function of part of the body after cancer surgery. Breast reconstruction after a mastectomy is an example of this kind of surgery.
Radiation Therapy
and/or chemotherapy. Radiation can be delivered externally -- where X-rays, gamma rays, or other high-energy particles are delivered to the affected area from outside the body -- or it can be delivered internally. Internal radiation therapy involves the placement of radioactive material inside the body near cancer cells. This is called brachytherapy.
Systemic radiation involves the administration of radioactive medication by mouth or intravenously. The radioactive material travels directly to the cancerous tissue. Radioactive iodine (I-131 for thyroid cancer) and strontium-89 (for bone cancer) are two examples of systemic radiation treatments.
Typically, external radiation is delivered 5 days a week over the course of 5 to 8 weeks. Other treatment regimens are sometimes used.
Chemotherapy Procedure
and/or relieve cancer-associated symptoms (such as pain).
Depending on the type of chemotherapy prescribed, the medications may be given by mouth, injection, intravenously (IV), or topically. IV chemotherapy may be delivered via a catheter or port, which is usually implanted in a blood vessel of the chest for the duration of the therapy. Sometimes chemotherapy is delivered regionally, directly to the area that needs treatment. For example, intravesical therapy is used to infuse chemotherapy directly into the bladder for the treatment of bladder cancer.
The chemotherapy regimen a patient receives depends upon the type and stage of the cancer, any prior cancer treatment, and the overall health of the patient. Chemotherapy is usually administered in cycles over the course of days, weeks, or months, with rest periods in between.
Other Treatments
In addition to surgery, radiation, and chemotherapy, other therapies are used to treat cancer. These include:Targeted or Biological Therapies
Hematopoietic Stem Cell Transplants
Angiogenesis Inhibitors
Cryosurgery
Photodynamic Therapy