This cancer begins in the ovaries, the twin organs that produce a woman's eggs and the main source of the female hormones estrogen and progesterone. Treatments for ovarian cancer have become more effective in recent years, with the best results seen when the disease is found early.
Ovarian Cancer Symptoms
 Bloating or pressure in the belly.
Bloating or pressure in the belly.- Pain in the abdomen or pelvis.
- Feeling full too quickly during meals.
- Urinating more frequently.
Risk Factor:
~ Family History
A
woman's odds of developing ovarian cancer are higher if a close
relative has had cancer of the ovaries, breast, or colon. Researchers
believe that inherited genetic changes account for 10% of ovarian
cancers. This includes the BRCA1 and BRCA2 gene mutations, which are
linked to breast cancer. Women with a strong family history should talk
with a doctor to see whether closer medical follow-up could be helpful.
~ Age
The
strongest risk factor for ovarian cancer is age. It's most likely to
develop after a woman goes through menopause. Using postmenopausal
hormone therapy may increase the risk. The link seems strongest in women
who take estrogen without progesterone for at least 5 to 10 years.
Doctors are not certain whether taking a combination of estrogen and
progesterone boosts the risk as well.
~ Obesity
Obese women have a higher risk of getting ovarian cancer than other women. And the death rates for ovarian cancer are higher for obese women too, compared with non-obese women. The heaviest women appear to have the greatest risk.Ovarian Cancer Screening Tests
 There
are two ways to screen for ovarian cancer before it causes symptoms or
shows up during a routine gynecologic exam. One is a blood test for
elevated levels of a protein called CA-125. The other is an ultrasound
of the ovaries. Unfortunately, neither technique has been shown to save
lives when used in women of average risk. For this reason, screening is
only recommended for women with strong risk factors.
There
are two ways to screen for ovarian cancer before it causes symptoms or
shows up during a routine gynecologic exam. One is a blood test for
elevated levels of a protein called CA-125. The other is an ultrasound
of the ovaries. Unfortunately, neither technique has been shown to save
lives when used in women of average risk. For this reason, screening is
only recommended for women with strong risk factors.Diagnosing Ovarian Cancer
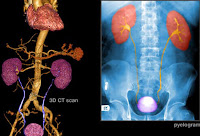
 Imaging
tests, such as ultrasound or CT scans (seen here), can help reveal an
ovarian mass. But these scans can't determine whether the abnormality is
cancer. If cancer is suspected, the next step is usually surgery to
remove suspicious tissues. A sample is then sent to the lab for further
examination. This is called a biopsy. Sometimes a sample taken with a
needle can also be used for diagnosis.
Imaging
tests, such as ultrasound or CT scans (seen here), can help reveal an
ovarian mass. But these scans can't determine whether the abnormality is
cancer. If cancer is suspected, the next step is usually surgery to
remove suspicious tissues. A sample is then sent to the lab for further
examination. This is called a biopsy. Sometimes a sample taken with a
needle can also be used for diagnosis.Stages of Ovarian Cancer
 The initial surgery for ovarian cancer also helps determine how far the cancer has spread, described by the following stages:
The initial surgery for ovarian cancer also helps determine how far the cancer has spread, described by the following stages:- Stage I : Confined to one or both ovaries.
- Stage II : Spread to the uterus or other nearby organs.
- Stage III : Spread to the lymph nodes or abdominal lining.
- Stage IV : Spread to distant organs, such as the lungs or liver.
The
vast majority of ovarian cancers are epithelial ovarian carcinomas.
These are malignant tumors that form from cells on the surface of the
ovary. Some epithelial tumors are not clearly cancerous. These are known
as tumors of low malignant potential (LMP.) LMP tumors grow more slowly
and are less dangerous than other forms of ovarian cancer.
Ovarian Cancer Survival Rates
Ovarian cancer can be a frightening diagnosis, with 5-year relative survival rates that range from 89% to 18% for epithelial ovarian cancer, depending on the stage when the cancer was found. But keep in mind that these odds are based on women diagnosed from 1988 to 2001. The treatments and outlook may be better for people diagnosed today. For LMP tumors, the five-year relative survival rates range from 99% to 77%.Ovarian Cancer Surgery
 Surgery
is used to diagnose ovarian cancer and determine its stage, but it is
also the first phase of treatment. The goal is to remove as much of the
cancer as possible. This may include a single ovary and nearby tissue in
stage I. In more advanced stages, it may be necessary to remove both
ovaries, along with the uterus and surrounding tissues.
Surgery
is used to diagnose ovarian cancer and determine its stage, but it is
also the first phase of treatment. The goal is to remove as much of the
cancer as possible. This may include a single ovary and nearby tissue in
stage I. In more advanced stages, it may be necessary to remove both
ovaries, along with the uterus and surrounding tissues.Chemotherapy
 In
all stages of ovarian cancer, chemotherapy is usually given after
surgery. This phase of treatment uses drugs to target and kill any
remaining cancer in the body. The drugs may be given by mouth, through
an IV, or directly into the belly (intraperitoneal chemotherapy.) Women
with LMP tumors usually don't need chemo unless the tumors grow back
after surgery.
In
all stages of ovarian cancer, chemotherapy is usually given after
surgery. This phase of treatment uses drugs to target and kill any
remaining cancer in the body. The drugs may be given by mouth, through
an IV, or directly into the belly (intraperitoneal chemotherapy.) Women
with LMP tumors usually don't need chemo unless the tumors grow back
after surgery.Targeted Therapies
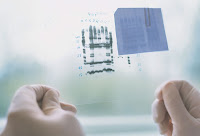
Researchers are working on therapies that target the way ovarian cancer grows. A process called angiogenesis involves the formation of new blood vessels to feed tumors. A drug called Avastin blocks this process, causing tumors to shrink or stop growing (seen in the illustration here). Avastin is approved for other cancers, but ovarian cancer researchers are still testing this therapy, which can have serious side effects.After Treatment:
~ Early Menopause
When
women have both ovaries removed, they can no longer produce their own
estrogen. This triggers menopause, no matter how young the patient. The
drop in hormone levels can also raise the risk for certain medical
conditions, including osteoporosis. It's vital that women have regular
follow-up care after being treated for ovarian cancer.
~ Moving On
Women
may find that it takes a long time for their energy to return after
treatments end. Fatigue is a very common problem after treatment for
cancer. Beginning a gentle exercise program is one of the most effective
ways to restore energy and improve emotional well-being. Check with
your health care team to determine which activities are right for you.
Risk Reducer:
~ Pregnancy
Women
who have biological children are less likely to get ovarian cancer than
women who have never given birth. The risk appears to decrease with
every pregnancy, and breastfeeding may offer added protection.
~ 'The Pill'
 Ovarian
cancer is also less common in women who have taken birth control pills.
Women who have used the pill for at least five years have about half
the risk of women who never took the pill. Like pregnancy, birth control
pills prevent ovulation. Some researchers think ovulating less often
may protect against ovarian cancer.
Ovarian
cancer is also less common in women who have taken birth control pills.
Women who have used the pill for at least five years have about half
the risk of women who never took the pill. Like pregnancy, birth control
pills prevent ovulation. Some researchers think ovulating less often
may protect against ovarian cancer.~ Tubal Ligation
 Getting
your tubes tied, formally known as tubal ligation, may offer some
protection against ovarian cancer. The same goes for having a
hysterectomy – removing the uterus while leaving the ovaries intact.
Getting
your tubes tied, formally known as tubal ligation, may offer some
protection against ovarian cancer. The same goes for having a
hysterectomy – removing the uterus while leaving the ovaries intact.~ Removing the Ovaries
 For
women with genetic mutations that put them at high risk for ovarian
cancer, removing the ovaries is an option. This can also be considered
in women over 40 getting a hysterectomy.
For
women with genetic mutations that put them at high risk for ovarian
cancer, removing the ovaries is an option. This can also be considered
in women over 40 getting a hysterectomy.~ Low-Fat Diet
 While
there is no definitive diet to prevent ovarian cancer, there is
evidence that what you eat can make a difference. In one recent study,
women who stuck to a low-fat diet for at least four years were less
likely to develop ovarian cancer. Some researchers report the cancer is
also less common in women who eat a lot of vegetables, but more studies
are needed.
While
there is no definitive diet to prevent ovarian cancer, there is
evidence that what you eat can make a difference. In one recent study,
women who stuck to a low-fat diet for at least four years were less
likely to develop ovarian cancer. Some researchers report the cancer is
also less common in women who eat a lot of vegetables, but more studies
are needed.